Introduction
Conditions affecting the bowel can often be tricky to diagnose.
Symptoms such as diarrhoea, constipation and bloating can have a number of causes.
Where these problems develop very quickly and pass after a short period, a viral or bacterial infection may be responsible.
However in cases where these symptoms return intermittently or persist, then further investigation may be required to determine what is causing them.
In some instances, there might not be just one cause, and the conditions contributing towards symptoms may overlap.
Different chronic conditions affecting the digestive tract can often have much in common; and in some instances, one condition might be related to or increase the risk of another.
Irritable bowel syndrome, as we’ve written before, is fairly common. When we spoke to the IBS Network, they told us that somewhere between 10 and 20 percent of all persons residing in Western countries would at some point display symptoms that adhere to the ‘diagnostic criteria’ for this condition.
Diverticular disease, in terms of outward symptoms at least, can appear similar to IBS. Bloating, constipation and diarrhoea are characteristics these two conditions share.
But are these two particular conditions related?
What is IBS?
Irritable bowel syndrome is characterised by food moving either too quickly or too slowly through the gut.
Rhythmic muscular contractions in the large intestine manage the speed at which food passes through. In those with IBS, it is thought that this rhythm is somehow disrupted.
This can result in a range of symptoms, including:
- Abdominal cramping
- Feeling windy and bloated
- Diarrhoea
- Constipation
- Mucus in the stool
Further symptoms that may occur as a result of IBS include:
- Acid reflux
- Feeling tired
- Headaches
- Nausea
- Going to the toilet to pass urine more frequently
- Muscular pain
Of course, not everyone will experience all of the above; the condition varies from person to person.
It’s not entirely understood what causes IBS, although higher gut sensitivity is widely thought to be the main instigating factor; certain foods, infections, inflammation and stress have all been cited as triggers.
Unsurprisingly, IBS can often be mistaken for other conditions. There is no definitive test to determine whether or not someone has IBS, so diagnosis typically consists of eliminating other conditions that can cause similar symptoms, such as infections, inflammatory bowel disease or food intolerances.
Treatment typically consists of making dietary changes to help alleviate symptoms, and to reduce the frequency and severity of flare-ups. However, which strategy a person adopts depends on their own individual case. For instance, reducing insoluble fibre can help with diarrhoea; whereas increasing soluble fibre and help with constipation. Practicing a low FODMAP diet can help to counter bloating.
Occasionally, certain medications can help to treat IBS. Antispasmodics work by relaxing the muscles in the bowel; whereas laxatives and antimotility drugs might be used to alleviate constipation or diarrhoea respectively.
What is diverticulosis?
Diverticulosis is characterised by the presence of diverticula. These are small pockets which form over time in the lining of the large bowel (typically in the lower descending section, known as the sigmoid colon). Diverticula are not uncommon and tend to develop with age. The NHS estimates that one in 20 will have them by the age of 40, and half of people will have them by the age of 80.
They develop as a result of the lining of the large bowel having to exert excess pressure to pass through stools. Diverticula form when weak spots appear in the muscle lining, and the mucosal layer on the inside of the bowel pushes through these.
Once more, no ultimately definitive answer has put been put forth as to why some people develop diverticula and others don’t, but there is thought to be a strong link between the formation of diverticula and a lack of dietary fibre.
In many instances, the presence of diverticula alone will not cause any significant problems. Only around one in four of those who have not had diarrhoea or abdominal discomfort will go on to develop symptoms.
Unsurprisingly then, it is entirely possible for someone to have diverticula for many years and not know.
What is diverticular disease?
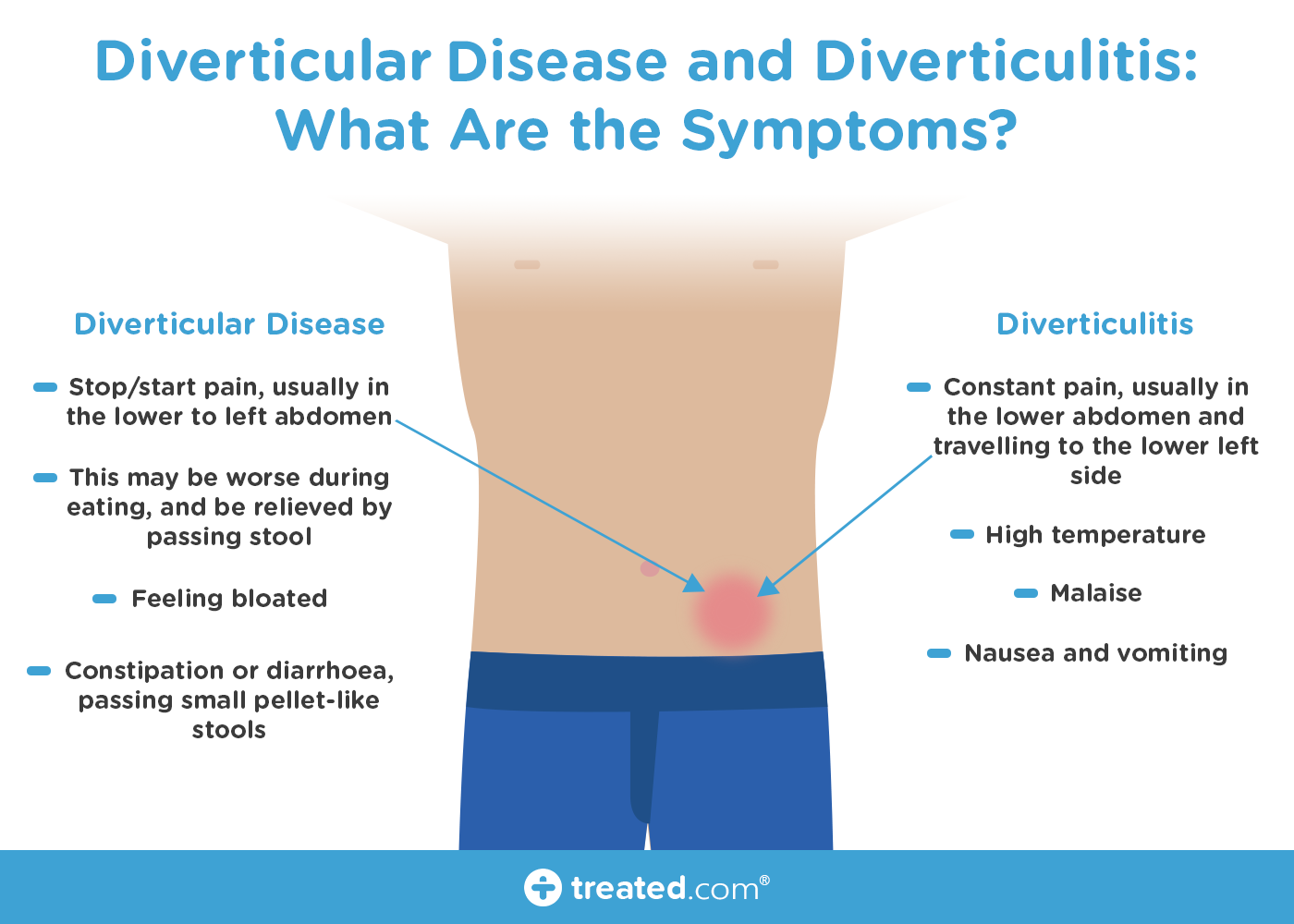
Where symptoms occur as a result of diverticula, this is known as diverticular disease. These symptoms might be:
- Stop/start pain, usually in the lower to left abdomen
- This pain may be worse during eating, and be relieved by passing stool
- Feeling bloated
- Constipation or diarrhoea, passing small pellet-like stools
Rarely, someone with diverticular disease may also pass dark or purple blood with their movements. This is a complication which will require hospital treatment. (Anyone who notices blood in their stools, purple or otherwise, should speak to their doctor as soon as possible.)
Diagnosis is made utilising a series of tests. Blood testing is commonly a first option. This will help doctors to eliminate the possibility of bowel cancer or IBD.
When these conditions have been ruled out, the presence of diverticula is often confirmed through an examination of the bowel (colonoscopy). This is where a camera on a tube is inserted into the rectum.
How diverticular disease is treated will be determined by how serious it is. In many cases, treatment can be administered at home. Paracetamol can help to reduce associated pain, and eating a high fibre diet can help to make bowel movements more consistent.
What is diverticulitis?
When one or several of the diverticula becomes infected, this can result in diverticulitis. This might occur due to a fragment of stool getting stuck in one of the pockets. The bacteria in the trapped fragment then transfers into the tissue and develops into an infection.
In diverticulitis, someone may have the symptoms of diverticular disease but also experience:
- Constant pain, usually in the lower abdomen and travelling to the lower left side
- High temperature
- Malaise (feeling unwell)
- Nausea and vomiting
According to the International Foundation for Functional Gastrointestinal Disorders (IFFGD), between one in five and one in seven people with diverticula (roughly 15-20 percent) will go on to develop diverticulitis.
Someone’s risk of developing diverticulitis is thought to be higher if they:
- Smoke
- Have had constipation for a long time
- Or are overweight or obese
Persons with an immediate family member who also has diverticular disease may also have a higher risk.
A diagnosis of diverticulitis might be made based on symptoms if a patient is known to have diverticular disease. But if they don’t, further testing may be required.
Treatment depends on how severe diverticulitis is. In milder instances, someone may be advised to take oral antibiotics to kill the infection, follow a liquid-only diet for a few days in order to let the bowel rest, and recover at home.
More serious cases (such as if the infection doesn’t improve after treatment at home, if complications are present or likely, or if oral antibiotics are not suitable) will require hospital admission. Antibiotics in this case may be administered via injections.
Where someone carries a very high risk of developing complications from diverticulitis, surgery to remove the section of colon affected by be necessary.
Are IBS and diverticular disease linked?
Diverticular disease can often be mistaken for IBS. Both conditions can produce similar symptoms such as bloating, pain, and changes in bowel frequency.
IBS is a long-term condition which goes through periods of flare-up and remission. But according to the IFFGD, it does not increase the risk of other gastrointestinal diseases (such as diverticulitis) developing.
However, recent research suggests that those who have had diverticulitis may be more likely to develop IBS symptoms.
A UCLA study in 2013 compared 1,102 post-infection patients with 1,102 matched controls over an average of 6.3 years; and found that those who had had diverticulitis were almost five times more likely to later be diagnosed with IBS than those in the control group.
The name the UCLA researchers proposed for this phenomenon was post-diverticulitis IBS (PDV-IBS).
Higher rates of anxiety were also observed in the post-infection group, which the lead researcher commented could trigger IBS symptom-inducing processes in the ‘brain-gut axis’.
Based on these findings, they noted that despite being an acute illness, diverticulitis may have the capacity to cause chronic ramifications.
It should be noted however that research into the association between these two conditions is still at a relatively early stage.
When to see a doctor
It’s important to report any significant changes in bowel habits to your GP, so that you can have the cause of them identified. Your doctor will be able to assist you in getting the treatment you need; whether it involves referral for further testing, or helping you to develop a diet plan to reduce or manage symptoms.




